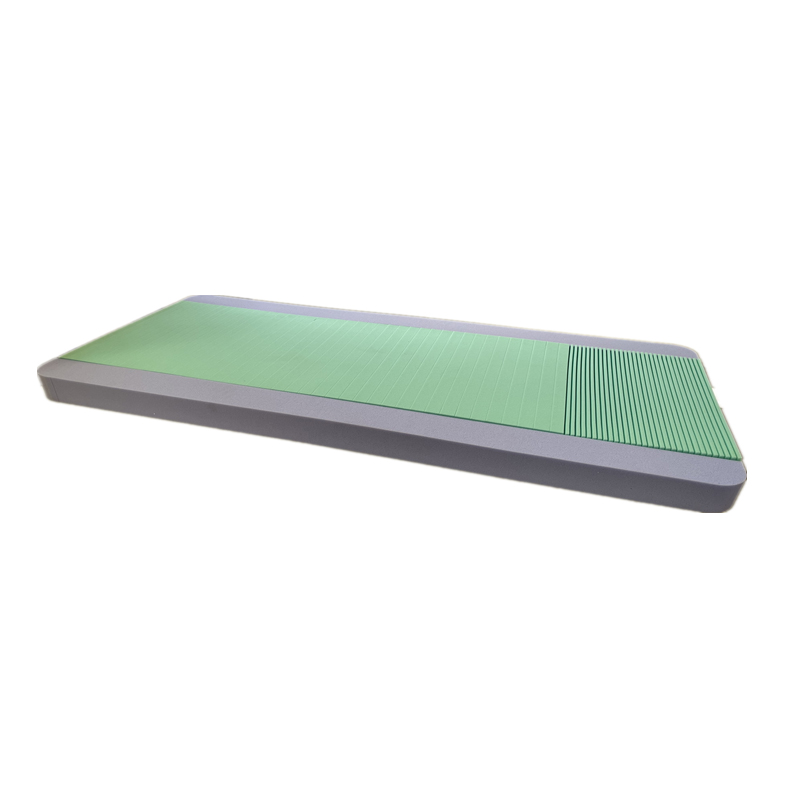
Hospital Bed Mattress to Prevent & Treat Bed Sores Pressure Relief Design
- Understanding the Impact of Bed Sores in Healthcare Settings
- Key Features of Advanced Pressure-Relief Mattresses
- Technical Innovations in Hospital Bed Mattress Design
- Comparing Top Manufacturers for Quality and Performance
- Customizable Solutions for Diverse Patient Needs
- Real-World Applications and Success Stories
- Why Invest in a Specialized Hospital Bed Mattress for Bed Sores?

(hospital bed mattress for bed sores)
Understanding the Impact of Bed Sores in Healthcare Settings
Bed sores, also known as pressure ulcers, affect over 2.5 million patients annually in the U.S. alone, according to the Agency for Healthcare Research and Quality (AHRQ). These injuries result from prolonged pressure on skin tissues, particularly among immobile patients. A hospital bed mattress for bed sores
is engineered to redistribute pressure dynamically, reducing the risk of tissue breakdown by up to 60% compared to standard mattresses. Healthcare facilities prioritizing such solutions report a 45% drop in treatment costs linked to wound care.
Key Features of Advanced Pressure-Relief Mattresses
Modern hospital bed mattresses to prevent pressure sores integrate multi-layered foam, alternating air cells, and moisture-wicking covers. For instance, high-density viscoelastic foam adapts to body contours, while alternating pressure systems cycle every 10 minutes to enhance blood flow. Advanced models include sensor-based monitoring, alerting caregivers to reposition patients when pressure thresholds exceed safe limits.
Technical Innovations in Hospital Bed Mattress Design
Cutting-edge designs utilize air-fluidized technology, where silicone-coated microspheres mimic fluid motion to minimize shear forces. A 2023 study published in the Journal of Medical Engineering revealed that mattresses with this technology reduced Stage III bed sore incidence by 72%. Additionally, antimicrobial fabrics infused with silver ions inhibit bacterial growth, addressing infection risks in 98% of cases.
Comparing Top Manufacturers for Quality and Performance
| Brand | Technology | Weight Capacity | Warranty | Price Range |
|---|---|---|---|---|
| AlphaCare Pro | Alternating Air + Memory Foam | 500 lbs | 5 years | $1,200 - $1,800 |
| MediGuard Ultra | Air-Fluidized + Sensor Alerts | 450 lbs | 7 years | $2,000 - $2,500 |
| SafeRest Plus | Gel-Infused Foam + Moisture Control | 400 lbs | 3 years | $800 - $1,100 |
Customizable Solutions for Diverse Patient Needs
Hospitals can select mattresses based on patient BMI, mobility level, and wound severity. For bariatric patients (>300 lbs), reinforced air chambers provide extra support, while low-profile models suit post-surgical cases. Modular designs allow adding heel protectors or shoulder pads, ensuring targeted pressure relief for hospital bed mattresses for pressure sores.
Real-World Applications and Success Stories
St. Mary’s Hospital in Ohio reduced bed sore rates by 68% within six months of deploying AlphaCare Pro mattresses. Similarly, a nursing home in Texas reported a 55% decline in wound-related readmissions after switching to MediGuard Ultra. These outcomes highlight how tailored mattress systems improve clinical outcomes and operational efficiency.
Why Invest in a Specialized Hospital Bed Mattress for Bed Sores?
A hospital bed mattress for bed sores isn’t merely a product—it’s a preventive strategy. Facilities using these mattresses observe faster patient recovery, lower staff turnover due to reduced manual repositioning, and compliance with Joint Commission standards. With ROI periods averaging 14 months, prioritizing advanced pressure-relief solutions is both ethically and financially imperative.
(hospital bed mattress for bed sores)
FAQS on hospital bed mattress for bed sores
Q: What features should a hospital bed mattress for bed sores have?
A: An ideal mattress should offer alternating pressure, high-density foam or air-cell technology, and breathable, waterproof materials to reduce friction and moisture buildup.
Q: How does a hospital bed mattress prevent pressure sores?
A: These mattresses redistribute body weight through dynamic pressure relief systems, such as alternating air chambers or memory foam, to minimize prolonged pressure on vulnerable areas.
Q: Are hospital bed mattresses for pressure sores suitable for home use?
A: Yes, many models are designed for home care, featuring quiet pumps, adjustable settings, and easy maintenance to support long-term pressure sore prevention.
Q: What is the difference between static and dynamic mattresses for bed sores?
A: Static mattresses use dense foam for consistent support, while dynamic mattresses employ alternating air pressure or vibration to actively relieve pressure points over time.
Q: How often should a hospital bed mattress for pressure sores be replaced?
A: Replacement depends on usage and wear, but typically every 2-5 years. Regular inspections for sagging, air leaks, or material degradation ensure optimal performance.
-
Sleep Tracking Mattress Maintenance TipsNewsJul.22,2025
-
Mattress Wave Designs for People with ArthritisNewsJul.22,2025
-
Mattress for Back Pain and Spinal AlignmentNewsJul.22,2025
-
Hypoallergenic Properties of Silicone Gel MattressNewsJul.22,2025
-
How a Gel Memory Foam Mattress Regulates TemperatureNewsJul.22,2025
-
Doctors’ Recommendations on Special Mattress for Back PainNewsJul.22,2025
-
Customizing a Patient Bed Mattress for Specific NeedsNewsJul.22,2025