bedsore prevention mattress product
Importance of Bedsore Prevention Mattresses in Healthcare
Bedsores, also known as pressure ulcers, are injuries to the skin and underlying tissue that occur primarily due to prolonged pressure on the skin. This issue is particularly prevalent in patients who are bedridden or have limited mobility. As the elderly population grows and more individuals require long-term care, the importance of preventing bedsores has become increasingly significant. One effective way to mitigate the risk of bedsores is through the use of specialized mattresses designed for prevention.
Understanding Bedsores
Bedsores develop when sustained pressure restricts blood flow to specific areas of the body, often over bony prominences such as the heels, sacrum, and elbows. The damage can range from mild skin redness to severe tissue damage that may require surgical intervention. Risk factors for developing bedsores include immobility, poor nutrition, dehydration, and moisture exposure due to incontinence. As healthcare providers strive to improve patient outcomes, the adoption of preventative strategies, including the use of specialized mattresses, is essential.
The Role of Prevention
Preventing bedsores is not only vital for patient comfort but also crucial for reducing healthcare costs associated with managing these injuries. The treatment of bedsores can be complicated and expensive, often requiring specialized care, wound management, and prolonged hospitalizations. According to the Agency for Healthcare Research and Quality (AHRQ), the average cost of care for a pressure ulcer patient is between $20,000 and $150,000, depending on the severity. Investing in preventive measures, such as pressure-relieving mattresses, can significantly reduce these costs.
Types of Preventive Mattresses
There are several types of mattresses designed specifically for bedsore prevention
bedsore prevention mattress product
1. Alternating Pressure Mattresses These mattresses utilize a system of air cells that inflate and deflate in a cyclical manner. This action redistributes pressure across the body, reducing the risk of prolonged pressure on any single area. Alternating pressure mattresses are often used in hospital settings but can also be beneficial for home care.
2. Low Air Loss Mattresses These mattresses provide a constant flow of air to maintain a slightly elevated surface that helps keep the skin dry and reduces moisture buildup. Moist skin is more vulnerable to bedsores, so keeping the skin dry is a crucial part of prevention.
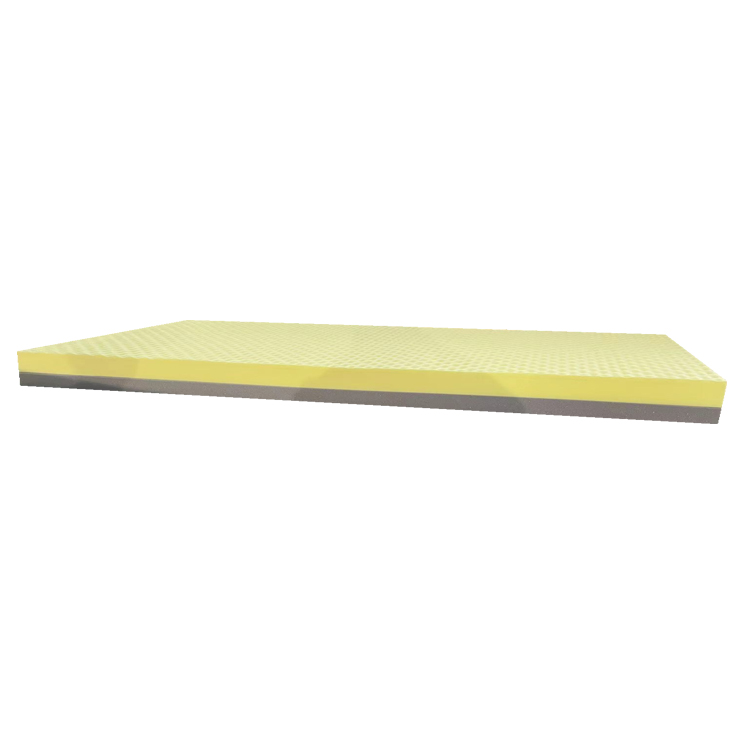
3. Foam Mattresses High-density foam mattresses offer excellent support and pressure distribution to reduce the risk of pressure sores. Some foam mattresses are designed with specific zones that provide tailored support for areas at higher risk for bedsores.
4. Gel Mattresses Gel mattresses combine gel technology with foam to enhance pressure relief and comfort. The gel helps to disperse body weight evenly and provides a cooler surface, minimizing heat buildup that might aggravate skin irritation.
Importance of Education and Training
While the type of mattress used is critical, educating healthcare providers and caregivers about the importance of regular repositioning and skin care is equally vital. Patients should be repositioned at regular intervals, typically every two hours, to alleviate pressure on vulnerable areas. Additionally, maintaining good nutrition and hydration plays a significant role in skin health and resilience.
Conclusion
The use of specialized mattresses for bedsore prevention is an important aspect of patient care in both clinical and home settings. With the potential to significantly reduce the incidence of pressure ulcers, these mattresses are essential tools in promoting patient comfort and enhancing overall health outcomes. As the healthcare landscape continues to evolve, ongoing education and investment in preventive measures are crucial to ensuring that every patient receives the best care possible. By prioritizing bedsore prevention through the use of advanced mattress technologies, healthcare providers can make a significant impact in improving the quality of life for those at risk. In the long run, prevention not only enhances patient well-being but also aids in reducing the costs associated with treating avoidable conditions.
-
Mattresses Designed for Back Pain ReliefNewsAug.08,2025
-
Innovative Wave Mattresses for Ultimate ComfortNewsAug.08,2025
-
High-Quality Mattresses for Hospital BedsNewsAug.08,2025
-
High-Quality Mattresses for Every NeedNewsAug.08,2025
-
Healthcare Foam Mattress: Sleep Better, Heal FasterNewsAug.08,2025
-
Cube Mattress for Daily ComfortNewsAug.08,2025
-
How Hospital Mattress Choices Directly Impact Patient Comfort and CareNewsAug.05,2025