Optimal Strategies for Effective Pressure Injury Management and Care
Best Practices in Pressure Injury Care
Pressure injuries, often referred to as bedsores or ulcers, represent a significant healthcare challenge, particularly for individuals with limited mobility. These injuries occur when sustained pressure on the skin compromises blood flow, leading to tissue damage. The consequences can be severe, culminating in infections, prolonged hospital stays, and increased healthcare costs. Therefore, understanding and implementing the best practices in pressure injury care is paramount in promoting patient wellbeing and recovery.
Prevention is Key
The cornerstone of effective pressure injury management is prevention. Regularly assessing at-risk patients is essential. This includes identifying those with limited mobility, poor nutrition, or underlying health conditions that might impair circulation. Utilizing validated risk assessment tools, such as the Braden Scale, helps healthcare providers determine individual risk levels, enabling targeted prevention strategies.
Changing a patient's position frequently is vital in alleviating pressure points. It is recommended that individuals be repositioned at least every two hours, but more frequent changes may be necessary for those at very high risk. Various methods, including turning, tilting, and using specialized cushions or mattresses, can distribute pressure more evenly across the body.
Nutrition and Hydration
Proper nutrition is critical for skin integrity and wound healing. Patients should receive a balanced diet rich in proteins, vitamins, and minerals, which play essential roles in tissue repair. Hydration also impacts skin health; adequate fluid intake can prevent the skin from becoming dry and more susceptible to injury. Healthcare providers should collaborate with dietitians to ensure that patients receive appropriate nutritional support tailored to their individual needs.
best pressure injury care
Early Detection and Management
Even with the best preventative measures, pressure injuries can still occur. Early detection is crucial for effective management. Healthcare providers should conduct regular skin assessments, particularly in high-risk areas such as the heels, sacrum, hips, and elbows. Any signs of redness, blistering, or skin breakdown must be addressed immediately.
Once a pressure injury is identified, it is essential to categorize it accurately, ranging from Stage I (non-blanchable erythema) to Stage IV (full-thickness skin loss). Appropriate wound care interventions should be initiated based on the stage. This includes keeping the wound clean, moist, and covered to facilitate healing while monitoring for signs of infection.
Patient and Family Education
Educating patients and their families about pressure injury prevention is vital. They should be informed about the importance of regular repositioning, skin care routines, nutrition, and the need to report any skin changes promptly. Engaging patients in their own care can significantly enhance outcomes and foster a culture of prevention.
Conclusion
In conclusion, best practices in pressure injury care encompass a comprehensive approach that includes effective prevention strategies, nutritional support, early detection, and ongoing education. By focusing on these aspects, healthcare providers can significantly reduce the incidence of pressure injuries, improve patient outcomes, and enhance the overall quality of care. Implementing these best practices is not only beneficial for patients but also vital for the healthcare system as a whole.
-
The Effect of Coconut Foam Mattress Breathability and Humidity Regulation on Improving Sleep QualityNewsJul.03,2025
-
How Wave Mattress Systems Improve Blood Circulation During ImmobilityNewsJul.03,2025
-
The Climate-Adaptive Sleep Revolution: Exploring the Benefits of Cooling Gel Memory Foam MattressesNewsJul.03,2025
-
Exploration of the Role of Coconut Foam Mattress in Preventing Bedsores in the ElderlyNewsJul.03,2025
-
Comparing Wave Mattress and Air Mattress: Which Is Better for Medical Use?NewsJul.03,2025
-
Analysis of Comfort and Environmental Performance of Natural Latex and Coconut Foam MattressNewsJul.03,2025
-
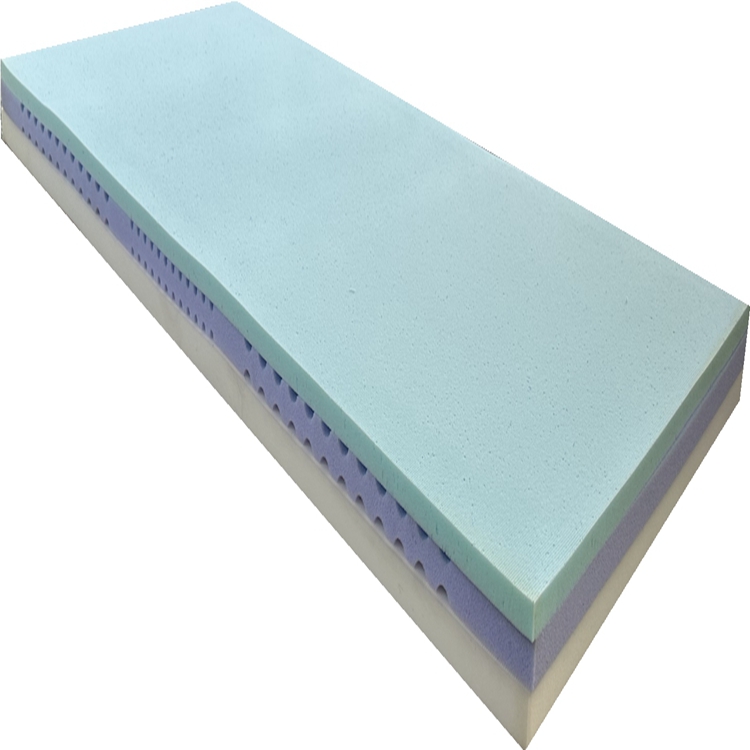
Multi-Layer Construction for Enhanced Performance in Gel Mattress PadNewsJun.24,2025