Understanding ODM Pressure Injuries and Their Impact on Patient Care
Understanding ODM Pressure Injury Causes, Prevention, and Management
Pressure injuries, also known as pressure ulcers or bedsores, are localized damage to the skin and underlying tissue, typically over bony prominences. They occur when there is persistent pressure, often in combination with shear and friction, which disrupts blood flow to the affected areas. In recent years, the concept of ODM (Ongoing Development and Management) pressure injury has gained attention, emphasizing a holistic approach to prevention and treatment.
Causes of Pressure Injuries
Pressure injuries are primarily caused by prolonged pressure on the skin, which can impede blood flow, leading to tissue ischemia and eventual necrosis. Several factors contribute to the development of these injuries
1. Immobility Patients who are bedridden or wheelchair-bound are at high risk as they may remain in one position for too long. 2. Moisture Excessive moisture from sweat or incontinence can weaken the skin and make it more susceptible to damage.
3. Nutrition Malnutrition and dehydration can compromise skin integrity and healing capacity.
4. Age Elders typically have thinner skin and reduced blood flow, making them more vulnerable.
5. Medical Conditions Chronic conditions like diabetes or vascular diseases can further impair skin health and healing processes.
The Role of ODM in Pressure Injury Management
The ODM approach integrates ongoing assessment, interdisciplinary communication, and continuous education to enhance the management of pressure injuries
. Here’s how this model is structured1. Assessment Regular and thorough evaluations of skin integrity are vital. Healthcare providers should utilize standardized tools to identify patients at risk for pressure injuries. Understanding the individual patient’s needs and risk factors helps tailor prevention strategies effectively.
2. Education Continuous training for healthcare staff, patients, and caregivers on the importance of pressure injury prevention strategies is crucial. This includes positions change schedules, proper skincare, and nutrition guidance.
odm pressure injury
3. Intervention Implementing effective interventions based on the assessment data is a key component of ODM. This may involve using pressure-relieving devices, optimizing nutrition, and enhancing moisture management.
4. Monitoring Ongoing monitoring ensures that interventions are effective. It allows for timely modifications to care plans based on patient progress or changes in condition.
Prevention Strategies
Prevention is at the core of pressure injury management under the ODM framework. Here are some key strategies
1. Regular Repositioning Changing a patient’s position at least every two hours can reduce pressure accumulation on vulnerable areas.
2. Support Surfaces Utilizing specialized mattresses and cushions that alleviate pressure can significantly lower the risk for at-risk individuals.
3. Skin Care Maintaining skin hygiene and using moisturizers can protect the skin from excessive dryness and moisture.
4. Nutritional Support Ensuring a balanced diet rich in proteins, vitamins, and minerals can enhance skin integrity and healing.
5. Patient Involvement Educating patients on the importance of movement and self-care can empower them to take an active role in their own prevention.
Conclusion
In conclusion, effectively managing ODM pressure injuries requires a comprehensive approach that emphasizes prevention, early detection, and continuous care. Through ongoing assessment, education, and adaptive interventions, healthcare professionals can significantly reduce the incidence of pressure injuries. By prioritizing skin health and implementing the ODM framework, we can improve patient outcomes and enhance the quality of care provided to those at risk.
-
The Effect of Coconut Foam Mattress Breathability and Humidity Regulation on Improving Sleep QualityNewsJul.03,2025
-
How Wave Mattress Systems Improve Blood Circulation During ImmobilityNewsJul.03,2025
-
The Climate-Adaptive Sleep Revolution: Exploring the Benefits of Cooling Gel Memory Foam MattressesNewsJul.03,2025
-
Exploration of the Role of Coconut Foam Mattress in Preventing Bedsores in the ElderlyNewsJul.03,2025
-
Comparing Wave Mattress and Air Mattress: Which Is Better for Medical Use?NewsJul.03,2025
-
Analysis of Comfort and Environmental Performance of Natural Latex and Coconut Foam MattressNewsJul.03,2025
-
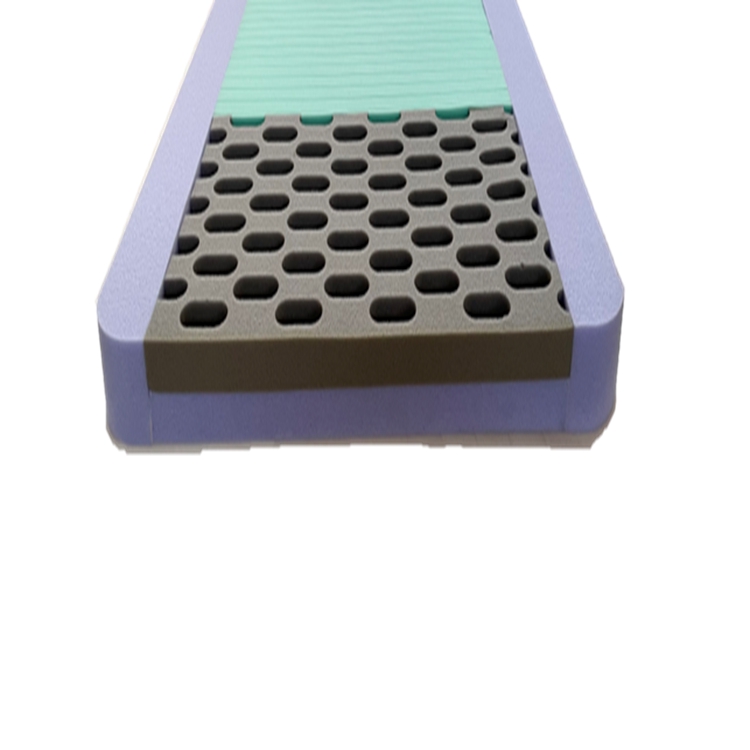
Multi-Layer Construction for Enhanced Performance in Gel Mattress PadNewsJun.24,2025