Best Hospital Bed Mattress for Bed Sores – Prevent Pressure Sores & Enhance Comfort
- Introduction: The significance of hospital bed mattress for bed sores
- Understanding Pressure Sores: Causes and Prevalence
- Technical Innovations in Hospital Bed Mattress to Prevent Pressure Sores
- Manufacturer Comparison: Features, Performance, and Value
- Custom Solutions for Diverse Patient Needs
- Real-world Application Cases and Outcomes
- Conclusion: Maximizing Comfort with the Right Hospital Bed Mattress for Bed Sores
(hospital bed mattress for bed sores)
Introduction: The Significance of Hospital Bed Mattress for Bed Sores
Hospitalized patients who are confined to bed for prolonged periods face a significant risk: the development of pressure sores, commonly referred to as bed sores or pressure ulcers. Hospital bed mattress for bed sores serves as a crucial intervention in this context. The selection of an appropriate mattress can dramatically reduce the incidence and severity of these painful wounds. According to the National Pressure Injury Advisory Panel, nearly 2.5 million patients in the United States develop pressure ulcers each year, costing the healthcare system over $11 billion annually. This blog explores how advanced mattress technologies, combined with informed selections and custom solutions, can transform patient outcomes, prevent complications, and optimize both care and cost.
Understanding Pressure Sores: Causes and Prevalence
Pressure sores, or decubitus ulcers, are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. They predominantly affect patients with limited mobility, especially those who are elderly, paralyzed, or recovering from surgery. The fundamental causes include pressure, shearing forces, friction, and moisture. A study published in The Lancet (2020) estimated that up to 17% of hospitalized patients in developed countries experience at least one pressure ulcer during their stay. These wounds typically develop at bony prominences, such as the sacrum, heels, and elbows, and can progress from superficial skin redness to deep, infected tissue loss if not managed promptly. The implementation of specialized hospital bed mattresses to prevent pressure sores is a frontline defense in patient care.
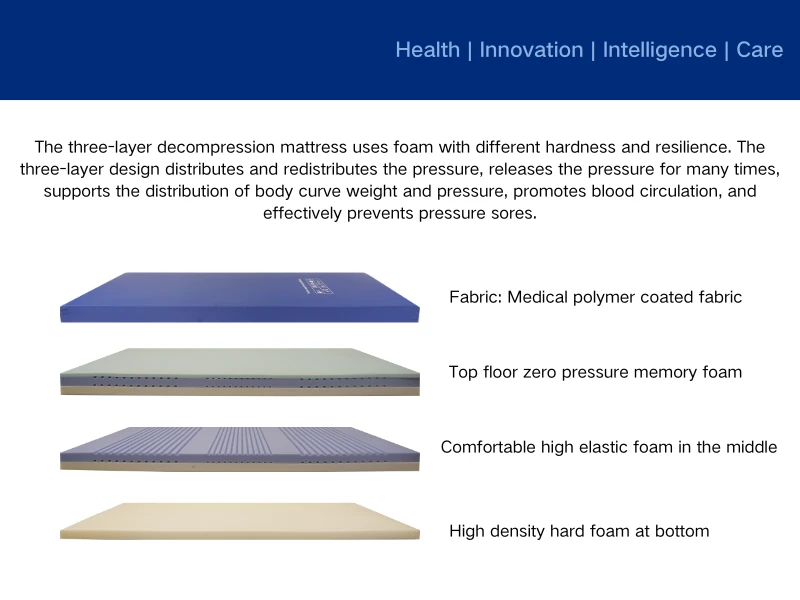
Technical Innovations in Hospital Bed Mattress to Prevent Pressure Sores
The field has seen a surge of technological advancements over recent years. Modern hospital bed mattress for pressure sores now integrate a multitude of sophisticated features designed to redistribute pressure, manage microclimate, and facilitate ease-of-use for caregivers. Key innovations include:
- Alternating Pressure Mattresses: These utilize powered air cells that cyclically inflate and deflate, minimizing prolonged pressure on any single area.
- Low Air Loss Mattresses: Engineered with micro-perforations to provide airflow across the skin surface, these help control moisture and temperature, key factors in pressure sore development.
- Gel-Infused Foam Mattresses: Combining viscoelastic foam with cooling gel, these mattresses conform to body contours and dissipate heat, while providing optimal pressure redistribution.
- Hybrid Mattresses: Offering a blend of static and dynamic support modes, these are adaptable to differing patient risk profiles and needs.
Manufacturer Comparison: Features, Performance, and Value
The market for hospital bed mattresses dedicated to pressure sore prevention is competitive, with several leading manufacturers delivering distinct technologies and values. The following table summarizes core attributes for well-known solutions:
| Manufacturer | Model | Core Technology | Pressure Redistribution (mmHg) | Smart Features | Max Load (lbs) | Warranty | List Price (USD) |
|---|---|---|---|---|---|---|---|
| Stryker | IsoFlex LAL | Low Air Loss | <12 | Microclimate Management, Weight Sensors | 500 | 5 yrs | 6,200 |
| Hill-Rom | Synergy Air Elite | Alternating Pressure | <15 | Automated Pressure Mapping | 550 | 3 yrs | 5,800 |
| Arjo | Auto Logic 200 | Hybrid | <14 | Individually Adjustable Cells | 440 | 4 yrs | 4,900 |
| Invacare | MicroAir MA55 | Low Air Loss + Alternating | <16 | Pump with User Controls | 350 | 2 yrs | 3,200 |
| Drive Medical | Med Aire | Alternating Pressure | <18 | Basic Visualization Indicators | 350 | 1 yr | 1,200 |
While Stryker and Hill-Rom focus on advanced features and higher capacities for high-acuity settings, brands like Invacare and Drive Medical offer budget-oriented options suitable for homecare environments. The choice hinges on clinical needs, budget, and desired feature set.
Custom Solutions for Diverse Patient Needs
The diversity among patients—ranging from pediatric to bariatric populations—necessitates tailored approaches. Facilities are increasingly demanding modular hospital bed mattress to prevent pressure sores that can adapt to individual risk profiles, body types, and co-morbidities. Manufacturers offer ranges with interchangeable components: variable density foams, adjustable air compartments, removable covers for infection control, and multi-zone pressure mapping. For example, heavier patients may require reinforced edge support and higher load ratings, while those prone to incontinence benefit from advanced wicking and antimicrobial materials. Clinical assessment tools such as the Braden Scale or Norton Scale are now integral to determining the optimal specification for each patient, ensuring that every bed mattress choice aligns precisely with clinical reality rather than generic use.
Real-world Application Cases and Outcomes
Implementation of pressure redistribution mattresses has driven measurable improvements in patient outcomes in real-world care settings. For instance, a 2023 quality improvement project in a 500-bed tertiary care hospital documented a reduction in new pressure ulcer cases from 13.6% to 5.1% after standardizing the use of alternating pressure mattresses for all high-risk admissions. Similarly, long-term care facilities have reported shorter healing times, reduced pain scores, and improved quality of life markers for residents following full deployment of pressure management mattresses. Home users and caregivers note less frequent need for repositioning, boosting comfort and dignity for patients. Furthermore, a large-scale meta-analysis published in International Wound Journal affirmed that dedicated hospital bed mattress for pressure sores can halve the risk of pressure ulcer formation compared to conventional support surfaces. These tangible results highlight the transformative power of investing in the right equipment.
Conclusion: Maximizing Comfort with the Right Hospital Bed Mattress for Bed Sores
Selecting a hospital bed mattress for bed sores is not merely about equipment, but about transforming care and preventing one of the most persistent complications in healthcare. From technical innovations and comparative manufacturer data, to the clinical reality of patient-centred customization and proven outcomes, the evidence is clear: deploying the correct mattress makes a substantial difference in patient well-being, recovery, and costs. Facilities and homecare providers are encouraged to assess their specific needs, reference comprehensive data, and recognize the critical role of technology and customization. Ultimately, a proactive choice in pressure management mattresses translates to fewer pressure sores, faster recoveries, more satisfied patients, and a more robust healthcare system.
(hospital bed mattress for bed sores)
FAQS on hospital bed mattress for bed sores
Q: What features should a hospital bed mattress for bed sores have?
A: A hospital bed mattress for bed sores should provide pressure redistribution, support, and airflow. Look for materials like memory foam or alternating pressure systems. These features help prevent the development of pressure sores.Q: How does a hospital bed mattress to prevent pressure sores work?
A: Such mattresses evenly distribute the patient's weight to minimize pressure on vulnerable areas. They may use advanced foams or air cells that adjust pressure dynamically. This helps reduce the risk of pressure sores.Q: Who should use a hospital bed mattress for pressure sores?
A: Patients with limited mobility or at risk of developing bed sores should use these mattresses. They are also ideal for those recovering from surgery or with chronic illnesses. The right mattress helps provide essential comfort and protection.Q: How do I clean a hospital bed mattress for bed sores?
A: Most hospital bed mattresses for bed sores come with a waterproof, wipeable cover. Use mild soap and water to clean the surface regularly. Always follow the manufacturer's cleaning instructions for best results.Q: Can a hospital bed mattress for pressure sores fit standard hospital beds?
A: Yes, most of these mattresses are designed to fit standard hospital bed sizes. Always check the dimensions before purchasing. Proper fit ensures maximum protection and patient comfort.-
Sleep Tracking Mattress Maintenance TipsNewsJul.22,2025
-
Mattress Wave Designs for People with ArthritisNewsJul.22,2025
-
Mattress for Back Pain and Spinal AlignmentNewsJul.22,2025
-
Hypoallergenic Properties of Silicone Gel MattressNewsJul.22,2025
-
How a Gel Memory Foam Mattress Regulates TemperatureNewsJul.22,2025
-
Doctors’ Recommendations on Special Mattress for Back PainNewsJul.22,2025
-
Customizing a Patient Bed Mattress for Specific NeedsNewsJul.22,2025