high quality pressure injury
Understanding and Addressing High-Quality Pressure Injuries
Pressure injuries, commonly known as bedsores or pressure ulcers, represent a significant concern in healthcare. These injuries occur when there’s prolonged pressure on the skin, typically in areas where bones are close to the skin's surface, such as the heels, elbows, and sacrum. Recognized for their potential to cause considerable pain and suffering, pressure injuries are also a major concern due to their association with increased healthcare costs and extended hospital stays. Because of this, understanding how to prevent, identify, and manage high-quality pressure injuries is imperative, especially for vulnerable populations like the elderly or individuals with limited mobility.
Definition and Stages
Pressure injuries are classified into several stages, ranging from Stage I (non-blanchable erythema) to Stage IV (full-thickness skin loss with exposed bone, tendon, or muscle). The severity of the pressure injury is crucial for determining the appropriate intervention and management strategies. High-quality pressure injuries can vary in complexity, from superficial damage to deep tissue injuries that can lead to serious complications if not treated effectively.
The specifics of each stage present unique challenges. Stage I injuries may appear as a persistent red spot on the skin, while more severe stages can involve significant tissue loss and require advanced interventions. Consequently, immediate identification and care are vital for preventing further deterioration.
Prevention Strategies
Prevention is the cornerstone of managing pressure injuries. Healthcare facilities have implemented a range of strategies to reduce the incidence of these injuries among patients. Key preventive measures include
1. Regular Skin Assessments Conducting thorough skin assessments to identify at-risk individuals can significantly reduce the likelihood of developing pressure injuries. Risk factors such as immobility, moisture, and nutritional status should be carefully evaluated.
2. Repositioning Changing the position of patients frequently is one of the simplest yet most effective methods of alleviating pressure. Repositioning should be carried out at least every two hours, though more frequent changes are often necessary for high-risk patients.
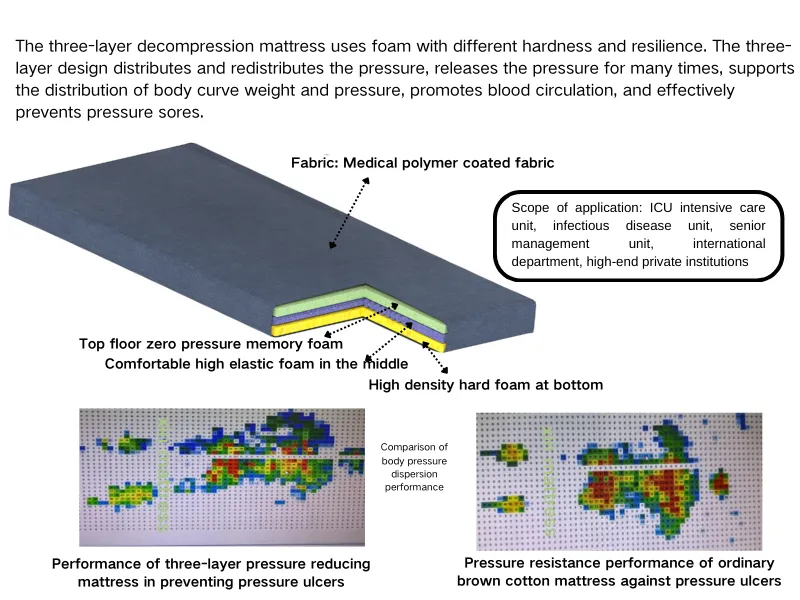
3. Support Surfaces Utilizing specialized mattresses and cushions designed to reduce pressure can greatly assist in pressure injury prevention. These support surfaces help distribute weight more evenly, thus minimizing localized pressure.
high quality pressure injury
4. Moisture Management Excess moisture can lead to skin maceration, increasing the risk of injury. Implementing strategies to manage moisture, such as using absorbent materials and keeping the skin clean and dry, is critical in prevention efforts.
5. Nutrition and Hydration Proper nutrition plays a vital role in skin integrity. Ensuring that individuals receive adequate hydration and nutrition can aid in healing and prevent the development of pressure injuries.
Management and Treatment
When a pressure injury does occur, prompt and effective management is essential. Treatment typically includes
1. Wound Care Maintaining a clean wound environment is critical. Regular cleansing, debridement of necrotic tissue, and application of appropriate dressings can facilitate healing.
2. Infection Control Identifying signs of infection early and implementing suitable interventions can prevent complications. Topical antibiotics and systemic antibiotics, if necessary, should be used judiciously.
3. Pain Management Addressing pain is crucial for patient comfort and promoting engagement in rehabilitation processes. Pain relief methods can range from pharmacological approaches to non-pharmacological interventions like repositioning and the use of pressure-relieving devices.
4. Patient Education Educating patients and caregivers about pressure injury prevention, identification, and management empowers them and encourages adherence to care plans.
Conclusion
High-quality pressure injuries represent a multifaceted challenge in healthcare delivery. Understanding the intricacies of prevention and management can make a significant difference in patient outcomes. With continued emphasis on risk assessment, proactive prevention strategies, effective treatment protocols, and education, healthcare providers can help mitigate the prevalence and impact of pressure injuries. Ultimately, prioritizing high-quality care in the management of pressure injuries aligns with a commitment to patient well-being and healthcare excellence.
-
The Effect of Coconut Foam Mattress Breathability and Humidity Regulation on Improving Sleep QualityNewsJul.03,2025
-
How Wave Mattress Systems Improve Blood Circulation During ImmobilityNewsJul.03,2025
-
The Climate-Adaptive Sleep Revolution: Exploring the Benefits of Cooling Gel Memory Foam MattressesNewsJul.03,2025
-
Exploration of the Role of Coconut Foam Mattress in Preventing Bedsores in the ElderlyNewsJul.03,2025
-
Comparing Wave Mattress and Air Mattress: Which Is Better for Medical Use?NewsJul.03,2025
-
Analysis of Comfort and Environmental Performance of Natural Latex and Coconut Foam MattressNewsJul.03,2025
-
Multi-Layer Construction for Enhanced Performance in Gel Mattress PadNewsJun.24,2025