custom pressure injury
Understanding Custom Pressure Injury Prevention and Management
Pressure injuries, often referred to as bedsores or pressure ulcers, are localized damage to the skin and underlying tissue, typically over a bony prominence. They occur when sustained pressure impairs blood flow, leading to tissue necrosis. With an aging population and increasing prevalence of conditions such as diabetes and obesity, understanding how to prevent and manage these injuries has become a crucial aspect of patient care.
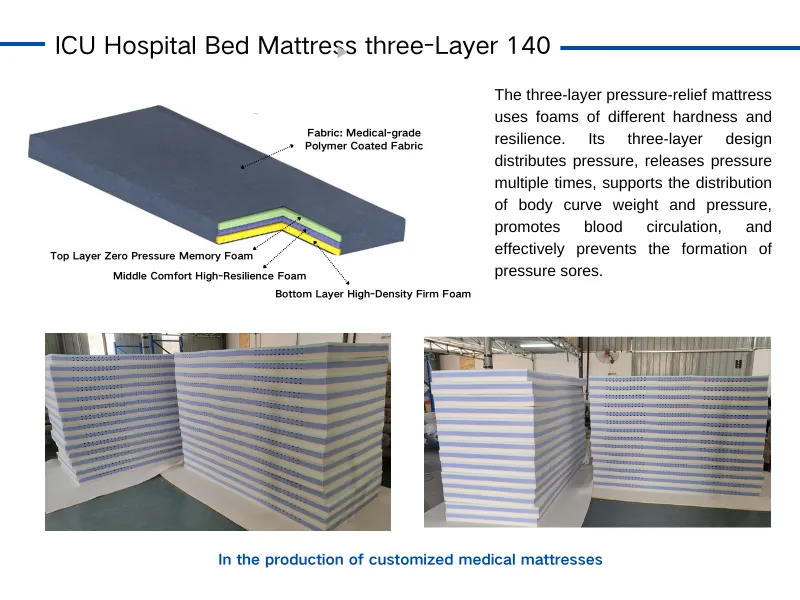
Custom approaches in pressure injury prevention focus on tailoring strategies to individual patient needs based on their risk factors. Key risk factors include immobility, incontinence, nutrition, and overall health status. For instance, patients who are confined to a bed or wheelchair require specialized interventions. Custom pressure relief surfaces, such as dynamic air mattresses or specialized cushions, can distribute weight more evenly and reduce pressure points. These surfaces adjust dynamically to the individual's movements, helping to maintain blood flow to vulnerable areas.
Furthermore, regular repositioning is essential. Healthcare providers should develop individualized repositioning schedules based on a patient’s condition. For example, changing a patient’s position every two hours can significantly reduce the risk of developing pressure injuries. In addition to physical repositioning, educating patients and caregivers about skin care and the importance of hygiene can also play a vital role in prevention.
custom pressure injury
Nutrition is another critical aspect of custom pressure injury management. Malnourished patients have a compromised ability to heal, making them more susceptible to injuries. Dietary assessments should be part of the custom plan, ensuring adequate intake of protein, vitamins, and minerals. Collaborating with dietitians can help create meal plans that support skin health and overall recovery.
Monitoring and early detection are also essential components of a custom strategy. Implementing regular skin assessments can identify early signs of pressure injuries, allowing for timely intervention. Advanced technologies, such as smart bandages that can monitor pressure and skin conditions, are emerging to assist healthcare providers in this effort.
In conclusion, custom pressure injury prevention and management involves a comprehensive approach that considers the unique needs of each patient. By integrating specialized surfaces, repositioning schedules, nutritional support, and advanced monitoring techniques, healthcare providers can significantly reduce the incidence of pressure injuries, ultimately enhancing the quality of care for vulnerable populations.
-
The Effect of Coconut Foam Mattress Breathability and Humidity Regulation on Improving Sleep QualityNewsJul.03,2025
-
How Wave Mattress Systems Improve Blood Circulation During ImmobilityNewsJul.03,2025
-
The Climate-Adaptive Sleep Revolution: Exploring the Benefits of Cooling Gel Memory Foam MattressesNewsJul.03,2025
-
Exploration of the Role of Coconut Foam Mattress in Preventing Bedsores in the ElderlyNewsJul.03,2025
-
Comparing Wave Mattress and Air Mattress: Which Is Better for Medical Use?NewsJul.03,2025
-
Analysis of Comfort and Environmental Performance of Natural Latex and Coconut Foam MattressNewsJul.03,2025
-
Multi-Layer Construction for Enhanced Performance in Gel Mattress PadNewsJun.24,2025